Delivering the Learning Advantage You Need to Succeed

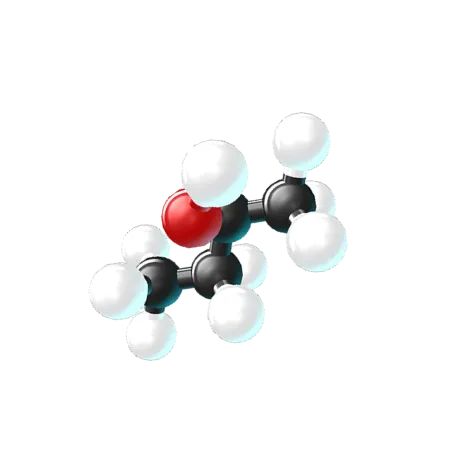
Put Your Students In the Shoes of Real Scientists
Offer students a glimpse into an exciting STEM career through simulations where they experience the thrill of solving real-world challenges.

Meet Students Where They Are
Develop self-efficacy with interactive experiences that reach students from all backgrounds. Provide a safe environment where students learn at their own pace.

Drive Success in Gateway Courses
Help your students learn STEM skills and concepts faster. Foster mastery with real-time feedback that improves grades and clears the path to completion.

Designed by and for Science Educators
Labster scientists incorporate continuous input from instructors to align seamlessly with curricula and effective teaching strategies.
Proven Impact in STEM Courses Across Academic Institutions

Labster helps teachers increase their students’ knowledge and test scores.
Research shows that low-knowledge students improve the most after using Labster, with a 24% increase in their test scores.
Source: BMC Study

80% of students said Labster made them more likely to continue enrolling in STEM classes.
Over 50% of first-year STEM students in the United States either change their majors or fail to earn their degree.
Source: LXD Study
.svg)
90% of students agreed that Labster provided opportunities for additional lab practice.
Undergraduate students typically require more time to complete lab experiments than provided.
Source: LXD Study
.svg)
Labster Ensures Your Success

Integrate With Your Existing LMS
Labster sets up your LMS integration or gets you started on our standalone platform.

Enhance Your STEM Curriculum
Labster works with you to match faculty with the most relevant virtual labs and course materials.

Receive Dedicated Ongoing Support
All subscriptions include support for faculty and students during and after deployment.
Bridging Gaps, Boosting Success: How to scale and personalize your teaching
This illuminating webinar unveils the incredible potential of personalized learning in today's rapidly evolving landscape.

October 5, 2023 12:00 PM

Join the Educator Community Campus Today
1,800+
Institutions
9M+
Played Simulations
900K+
Active Students